Meet DAN
Voice Enabled
Intelligent Claim Denial Analysis Powered by AI
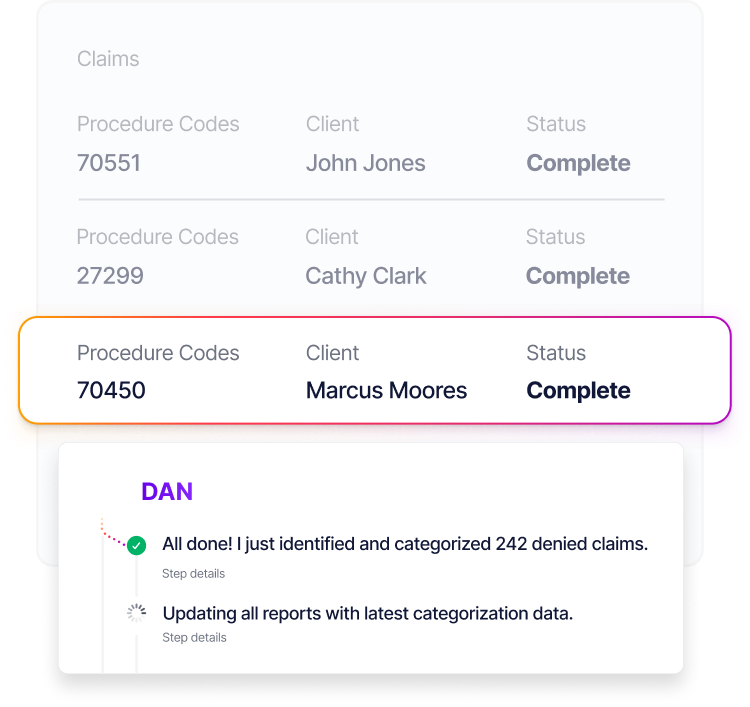
Every claim denial is analyzed and categorized automatically, providing insights to accelerate your revenue recovery process.
.png)
Intelligent Denial Routing
Fix denials at the source before they impact revenue
DAN automatically identifies the root cause of each denial and routes issues to the appropriate team member or process for resolution. Missing authorizations go to your prior auth team, coding errors are flagged for your coders, and eligibility issues are routed back to verification. What used to require manual triage now happens instantly.

Real-Time Denial Insights
Understand denial patterns with actionable data
Real-time analytics provide a clear view of denial patterns, helping RCM teams to address recurring issues and optimize processes. This proactive approach reduces denial rates and supports faster revenue recovery, keeping your cash flow steady.
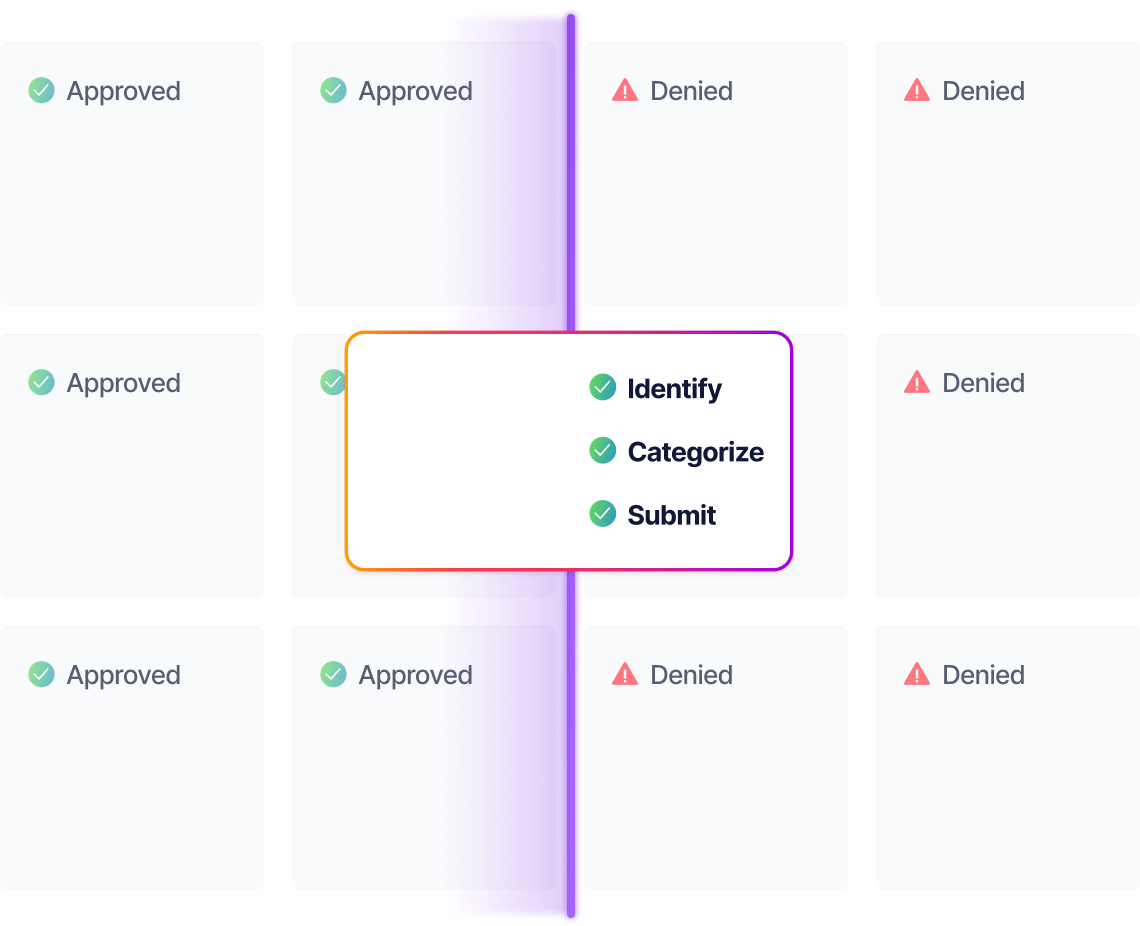
Intelligent Denial Categorization
Prioritize denials by impact and resolution complexity
DAN uses AI to analyze each claim denial, categorize by reason code and resolution priority, and provide clear action plans for your team. Streamline your denial workflow and focus efforts where they'll have the greatest financial impact.
All Features
Description

Voice Enabled
Voice enabled DAN can follow up on denied claims seamlessly, even over the phone, automating appeals and reducing delays in payment recovery.

Detects Underpayments
Identifies patterns indicating potential underpayments by analyzing payer payment trends against contracted rates and historical payment data.

Intelligent Denial Categorization
Uses AI to categorize denials by complexity, priority, and required actions, enabling teams to work most efficiently.

Batch Analysis for High Volumes
Efficiently analyzes large volumes of denials, providing insights and recommendations even as claim volumes scale up.

Appeals Generation
Automatically drafts appeal letters with relevant clinical documentation and payer-specific requirements, giving your team a complete starting point for appeals.

Scalable Across Practices
Supports practices of all sizes, maintaining analysis accuracy and insight quality as your organization grows.

Customizable Alerts & Notifications
Sends real-time updates on critical denial patterns, compliance alerts, and high-priority cases, keeping your team informed and proactive.

Denial Code Analysis
Analyzes denial patterns to identify root causes, like missing data or incorrect codes, providing clear resolution pathways.

Integrated System Compatibility
Seamlessly connects with EHRs, PMS, and financial systems, pulling denial data for comprehensive analysis.

Real-Time Reporting & Insights
Offers immediate access to denial trends, resolution recommendations, and workflow efficiency metrics.

Automated Workflow Recommendations
Provides specific action plans for each denial type, helping teams resolve issues faster and more consistently.

Cara Perry
SVP of Revenue Cycle Management,
Signature Dental Partners
It's like training a perfect employee, that works 24 hours a day, exactly how you trained it.
Cara decreased days sales outstanding to 45% below industry standards
One Platform, Endless Integrations
Thoughtful's AI agents can operate all of your systems.







